Case 28: Nina
Social, cultural and historical context
Nina, aged 61, is white British, and lives alone in sheltered accommodation. She was once married but divorced some years ago. She has lived in this flat for 12 months. Before this, she lived in other sheltered accommodation where she was not happy because she had a ground floor flat where she did not feel secure. Children threw stones at her window and other residents were shouting and swearing. None of the other residents spoke English and there were a lot of alcoholics. Prior to this she had been homeless and living in hostels. At one time, she was living on the streets. She still visits an NHS clinic for the homeless once a month. Between 2005 and 2008, she lived with a friend in the USA. She does voluntary work with an organisation that manages hostels for the homeless. In summer 2012, she had paid employment at the Olympic Games.
Participant's experience of ageing and ill health
Nina has type 2 diabetes that was diagnosed when she lived in the USA. She currently takes tablets for the diabetes but the nurse at the clinic sometimes says she is "close to needing to take insulin". She has been advised by the nurse to lose weight. She knows this is a problem and is not sure what to do about it. She has tried lots of different diets. The nurse has encouraged her to exercise but Nina feels this is out of the question because of the pain in her right leg and down her right side, the result of a car accident 18 years ago.
Nina goes to the 'homeless' clinic once a month on Wednesdays for a check on things like her blood sugar, blood pressure, cholesterol and weight. She is up by 7 am and gets to the clinic at 8 am, one hour before it opens:
"First in, first seen. … Get there an hour before it opens. If you don't get there before, you could be sat in there for hours. Because I used to go 15 minutes before, got there, and the queue was half way down the road"
Her blood sugar control is checked every 3 months at the clinic. It used to be every month. Nina does not understand what she sees on the nurse's computer screen "…but I just look to see what it says". Nina is worried about her blood sugar levels because she cannot afford the strips to monitor her blood sugar. She is frustrated that the NHS doesn't provide the equipment so she can manage her blood sugar and possibly prevent the need to go on to insulin injections.
"If I had all the stuff, yes I could test myself to check my blood is where it should be. So I can see if I am eating something too sugary and stop."
Although Nina does take her medication for diabetes, she does not control her diet. She always feels confused when the nurse tells her to carry on with what she is doing because she does not know what it is that she does to keep it under control.
"I can eat five bars of chocolate every day and keep the sugar level stable. I don't know how, and she [the nurse] says keep doing what you're doing. I don't know what or how…. I love chocolate. But then another time the bar will be in there [drawer] for weeks. My whole thing is very very weird all together as far as I'm concerned."
As well as medication for diabetes, Nina also takes painkillers, tablets to help her sleep, and to reduce her cholesterol level. She has never forgotten to take her medication. It is the first thing she does in the morning. She leaves a glass of water out on the worktop overnight (covered with a piece of paper in case of flies). If the paper is still on top of the cup, that reminds her to take her medication. The tablets are too important for her to miss, and so she keeps to her regimen. However, on mornings when she has rushed to work, she worries whether she had taken her medication, especially the diabetes tablets. There have been a few occasions when she has arrived at work and rushed back home to see if she had taken the tablets.
Nina has been advised by the nurse to lose weight, but cannot think what she can cut down on. She insists that she has tried various diets, and none have worked. This issue came up during her last clinic appointment, but Nina is confused as to why she has gained weight, and so cannot think how she is going to lose it:
"[The nurse] said everything has gone wrong, everything has gone up here. It should be down here – that's on the cholesterol, high blood pressure, sugar levels, whatever, other things. There's so many of them I just sit there and go 'ahh yeah'. And I see the number go up and then 'ohh no'. I've got to try and lose weight, for some unknown reason I have gone from 12 stone to 14 and a half stone."
Nina bought weight loss tablets off the Internet. The tablets also come with some patches (like nicotine patches). According to the instructions, these suppress appetite. The instructions state that the patches should be placed in the area where you want to lose weight.
The nurse suggested exercise, but Nina cannot exercise due to pain in her back and legs ("I can't walk a lot, my legs won't let me. If I start walking I get in more agony than anything else"). She would like to get a cycling machine, but doesn't know how to get one and she doesn't want to go to a gym, partly because she is self-conscious ("I don't know where you can go for the gym, and I feel a bit of a twit going like this").
People in this participant's life
Nina has a close friend, Annie, in the North of England where she lived previously. She visits Annie and her three daughters at Christmas. She has three female friends who live in the sheltered accommodation.
Nina has a friend, Mike, whom she met when she was homeless. He has very poor health (TB, "weak lungs", emphysema). He recently stayed with her briefly after he had had a foot operation. He left in the middle of the night and she hasn't seen him since. She's worried, about this.
What matters to this participant?
Nina's voluntary work is important. Her weekly routine centres on her work at the housing association that manages hostels for the homeless. She works there Mondays, Tuesdays and Thursday from 9 am to noon. She works on reception – letting people in, seeing which hostel they want (different hostels have different rules, such as no alcohol) and does routine checks at different hostels. She is leads the Maintenance Advisory Panel (MAP). This involves her going to various hostels in the area and checking for damage, cleanliness and health and safety issues in all the rooms and recording anything that needs to be sorted out. After her voluntary work Nina is exhausted ("I conk out").
On Saturdays Nina sometimes volunteers at a homeless feeding station. There the homeless can have a shower, pick some clothes, see a health professional and have some breakfast and lunch. She has to get there at 6am to get all the tea and cups ready for when everyone arrives. On Sundays she goes to a community centre for a service with the Salvation Army. Often they go out to collect money in London.
Nina's friendship with Annie is very important to her. She refers to Annie as "my daughter" and to Annie's three daughters as "my girls". She saves the £10 Tesco vouchers she gets for her voluntary work for Annie to use over Christmas when Nina is staying with her. Usually they are in regular contact over Facebook.
Social contact in the sheltered accommodation is important to Nina. On one occasion when the researcher visits, the residents are having a barbeque. Nina does not want to miss this because these gatherings are rare. There is a communal room and garden in the property but residents rarely gather there. Nina speaks mainly with her three chosen friends. The communal room is large but never used.
Nina's weight problem matters to her, because she does not want to go onto insulin. She is hoping that the diet tablets and patches she purchased from the Internet will make a difference over the next month. Nina is seeking some education on what to do or eat to manage her weight. She wants specific instructions for a diet that she can follow. She looks on the Internet but finds it hard to trawl through it all, find information that is relevant to her and to trust the content.
"I go on the Internet and it automatically takes you to America, and I'm using Yahoo UK. So when you're trying to find out where to go, what to do, you're not getting anything English….You want it for England. Say special patches or something. [… ] I know I am type 2 [diabetes], I know I am near enough type 1, but what I want to know is why and how to cut it down and stop it. And then you see things on here [internet] saying 'Go to this place, or that place, and take this and take that, and it will stop diabetes all together'. But if that was the case why are there so many millions of people who have got diabetes".
Technologies in Nina's home and life
Nina says she has no telehealth and few telecare technologies. She thinks she just has the standard pull cord setup in the sheltered accommodation where she lives. She says she does not have a pendant alarm and doesn't need one. The researcher points out to her that there is a pendant alarm hanging from the alarm unit in the hallway, but she has never noticed it.
Nina's main piece of technology is her laptop, which she uses to search the Internet and use email, Facebook, and more recently her bank account. She also uses it to play games, which she downloads from the Internet ("They keep me going"). She uses an Internet USB/dongle, which is £15.99 a month.
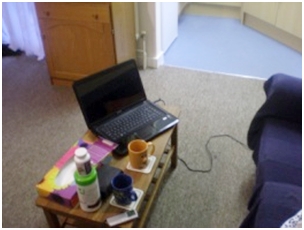
Nina's laptop
Nina has a new touch screen mobile. Annie does not have a landline and it's too expensive to call her mobile. Nina recalls a "horrible" incident when she was told that her mobile phone calls were free to other mobiles after 7 pm. She called lots of people after 7 pm, and then received a £100 phone bill. Nina has an old landline phone handset. She doesn't use this phone anymore, but has hung onto the handset as there is a game on it that she still likes to play.
Nina has a camera and she shows the researcher the photos a friend from work downloaded them for her and emailed them to her. However, she doesn't know how to put them onto her computer, and she doesn't want to have to keep going into her email account to view them. The researcher shows her how to download the attachments.
Materiality and capability
Nina manages to look after herself very well in day-to-day life. Whilst the pain in her side and leg stops her exercising, it does not affect her independence in any other way. She has no problems washing, dressing or managing the home. She has some difficulty remembering whether she has taken her diabetes medication despite using a dosette box.
Nina can read enough to follow emails, but she wasn't able to read or understand the information leaflet that came with the diet product she bought from the Internet. This was partly because the print was too small.
Nina's daughter showed her how to use a computer about 18 years ago. "I didn't want to know initially. She was teaching me this and teaching me that, and I've never been off the computer or laptop since. I would be lost without one."
Whilst Nina uses her laptop for online banking, she still asks the bank to print out the statements so she can see what she needs. There have been a few incidences when she has not had the money to pay bills, and so she wants a written list of how much she has to pay, and when it needs to be paid:
"Because I got fed up, like with SKY, they wanted their money and it wasn't in the bank. And I put it in the bank, but for some unknown reason, somehow or other it didn't stay in the bank. So I was in a mess time and time again. It annoyed me."
Real incidents of using (or choosing not to use) an ALT
Nina has never used the pull cords in her flat. She finds them a bit of a nuisance. She has tied one cord up out of the way and hidden another behind bookshelves, though she recognises that there may be a time when she might need them as her legs can get bad. The one by her bed may be useful, she thinks, if she woke up unable to get up, but the one in the hallway would be too high to reach if she had a fall. She doesn't know where the call goes to when they are pulled. She doesn't feel she needs the pendant alarm that the researcher pointed out to her.
On one occasion, she asked a friend, Jenny (who lives downstairs) if she could press her pendant alarm because someone was trapped in the lift:
"I went down to see if she had her button, and if she could call someone because somebody was stuck in the lift. He was panicking in there, and then it went dead silent, so she pressed something or other…a voice came up on her wall and they said 'Yes what's happening?' They said 'somebody will be on their way'…I haven't a clue [who it was], it went to whoever it went to."
Comment
This case, of one of the youngest and least disabled participants in our study, illustrates a person with deteriorating chronic illness who has some assistive technologies and the capability to use them, but whose situation is made precarious by low health literacy and limited social support.
Even though Nina has spent time homeless and living on the streets, she is perfectly comfortable using computer technology – something she learnt in order to keep in touch with distant friends. However, she appears to have limited capability to track down and understand health information. Importantly, nobody is guiding her in this regard so she is 'flying solo'.
Whilst Internet technology could support Nina to gain an understanding of her condition, grasp the principles of dietary control and identify appropriate foods, she surely needs human input of one sort or another – either from professional educators or peers with diabetes from whom she might learn.
Nina has no equipment to monitor her blood sugar levels because she can't afford the strips, which would be £20 to £30 per month, to use the blood sugar monitor. Arguably, it is a false economy not to allow Nina the opportunity to monitor her blood sugar levels and possibly avoid deterioration of her conditions. An alternative argument is that Nina's control would be no better even if she were given the strips for free, since a limited understanding of the condition may not enable her to reflect on the readings and adjust her diet accordingly. Nina may, however, be a good candidate for a technology-based medication reminder system.
Nina uses a mobile broadband dongle with her laptop costing her £15.99 per month. Free WiFi in the sheltered accommodation would reduce the cost of using the technology for Nina and may encourage others to use computer technology to enhance their social networks.
Despite being able to use computer technology for online banking, Nina still has to ask the bank staff to print off statements to help her sort out her finances. Using the technology to access her bank account is not difficult for Nina, but having sufficient economic resources and managing them is difficult. Nina also illustrates the challenge of health literacy. She sees the test results on the nurse's computer screen but cannot understand them. A frequent clinic attender, Nina is unlikely to transfer smoothly to a remote relationship mediated by a computer link.